Antibiotic misuse poses a threat
Antibiotic misuse poses a threat
Ultimately, AMR is not just a medical problem, but a social, economic, and policy challenge. Responsible use of antibiotics today will determine whether future generations will have effective treatment options.
- Antibiotic misuse is creating a serious AMR crisis.
- Shared responsibility of the government, IMA and society is necessary.
- The spread of antibiotic residues in the environment is a matter of concern.
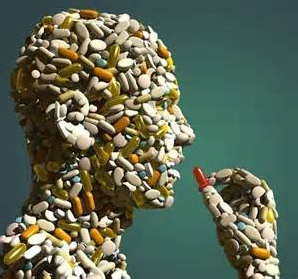
Antimicrobial resistance (AMR) is one of the most serious, yet least understood, public health crises facing the world today. This problem is gradually undermining the basis of treatment. When bacteria, viruses, fungi, and parasites become resistant to drugs, even common infections can become life-threatening. The impact is even more profound in developing countries like India, where the infection burden is high and health resources are limited.
In 2019, approximately 5 million deaths worldwide were linked to AMR. If we don’t address and control it now, this number could reach 10 million annually. This crisis is also dangerous because its symptoms appear gradually, and by the time treatment becomes ineffective, it may be too late.
Prime Minister Modi has consistently emphasized that antibiotics should not be used without medical advice. This appeal is significant because many illnesses, such as the common cold, fever, or viral infections, resolve on their own, and antibiotics play no role. Despite this, unnecessary and irrational use of medications has become commonplace in our society. This indiscriminate use allows microorganisms to become more resistant, potentially rendering life-saving medications ineffective in the future.
This situation is worrying because new antibiotics are not being developed at a pace commensurate with the rate at which microorganisms are becoming resistant. No major new class of antibiotics has emerged in the past two decades. Developing a new antibiotic is a lengthy, complex, and extremely expensive task, taking 15 to 20 years. Despite significant investment, the economic returns remain limited. This is why pharmaceutical companies shy away from major investments in this area.
The government has developed a multi-pronged approach to combat AMR. Under the national action plan, surveillance systems are being strengthened to monitor drug resistance trends in a timely manner. Controlling over-the-counter antibiotic sales, antimicrobial stewardship programs in hospitals, and promoting laboratory-based testing are steps in this direction. Efforts to control antibiotic use in animal husbandry, agriculture, and fisheries are also part of the government’s One Health strategy, which recognizes the interconnectedness of human, animal, and environmental health.
The Indian Medical Association also plays a key role in this fight. The IMA is actively involved in raising awareness among physicians across the country about AMR, promoting responsible prescribing, and communicating the right message to the general public. The IMA’s AMR Committee has consistently warned that antibiotic misuse not only complicates treatment but also poses a threat to entire generations. Antibiotics are most commonly misused to enhance the growth of animals, fruits, and vegetables, rather than to protect human health.
A serious aspect of this crisis also relates to the environment and rivers. Rivers, ponds, and groundwater are becoming contaminated with AMR due to human activities, hospital waste, industrial waste, antibiotic residues from farms, and animal feces. Experts are constantly warning about the presence of resistant bacteria and antibiotic residues in many rivers. These are becoming active carriers of AMR, transmitting the threat to humans through water, soil, and the food chain. This contaminates the food chain and contaminates water sources. Common water purification systems are not capable of filtering AMR, allowing it to enter the human body through water.
The fight against AMR is not just the responsibility of doctors or the government, but of society as a whole. Unless ordinary citizens understand this threat, policies and regulations will have limited impact. Antibiotics should only be used on prescription from a qualified physician. Adherence to the full dosage and correct duration of medication is essential. Restrictions on over-the-counter sales must be strictly enforced.
Hygiene, sanitation, safe water, and widespread vaccination are the most effective means of preventing infection. Improved diagnostic facilities can ensure the right medicine is given for the right disease. Increasing government investment and incentives for antimicrobial research and innovation is crucial. Ultimately, AMR is not just a medical problem, but a social, economic, and policy challenge. Responsible use of antibiotics today will determine whether future generations will have effective treatment options.